Trefoil Family Factor Peptide 1—A New Biomarker in Liquid Biopsies of Retinoblastoma under Therapy
Abstract
:Simple Summary
Abstract
1. Introduction
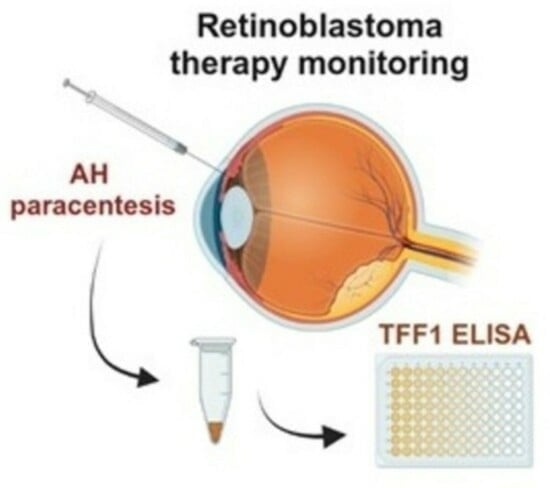
2. Materials and Methods
2.1. Human Retinoblastoma Tumor, Aqueous Humor, and Blood Samples
2.2. Primary RB Cell Culture
2.3. Blood Serum Concentration and TFF1 ELISA Analysis
2.4. Immunohistochemistry and Immunofluorescence Stainings
2.5. Statistical Analysis
3. Results
3.1. Soluble TFF1 in Aqueous Humor of RB Patients Is Secreted by RB Tumor Cells
3.2. Analysis of Soluble TFF1 Secretion in AH and Blood of RB Patients under Therapy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, J.; Ottaviani, D.; Sefta, M.; Desbrousses, C.; Chapeaublanc, E.; Aschero, R.; Sirab, N.; Lubieniecki, F.; Lamas, G.; Tonon, L.; et al. A high-risk retinoblastoma subtype with stemness features, dedifferentiated cone states and neuronal/ganglion cell gene expression. Nat. Commun. 2021, 12, 5578. [Google Scholar] [CrossRef] [PubMed]
- Singh, H.P.; Wang, S.; Stachelek, K.; Lee, S.; Reid, M.W.; Thornton, M.E.; Craft, C.M.; Grubbs, B.H.; Cobrinik, D. Developmental stage-specific proliferation and retinoblastoma genesis in RB-deficient human but not mouse cone precursors. Proc. Natl. Acad. Sci. USA 2018, 115, E9391–E9400. [Google Scholar] [CrossRef] [PubMed]
- Dimaras, H.; Corson, T.W. Retinoblastoma, the visible CNS tumor: A review. J. Neurosci. Res. 2018, 97, 29–44. [Google Scholar] [CrossRef]
- Bornfeld, N.; Lohmann, D.; Bechrakis, N.E.; Biewald, E. Retinoblastom. Ophthalmologe 2020, 117, 389–402. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.R.; Kaliki, S. Retinoblastoma: A Major Review. Mymensingh Med. J. 2021, 30, 881–895. [Google Scholar]
- Bouchoucha, Y.; Matet, A.; Berger, A.; Carcaboso, A.M.; Gerrish, A.; Moll, A.; Jenkinson, H.; Ketteler, P.; Dorsman, J.C.; Chantada, G.; et al. Retinoblastoma: From genes to patient care. Eur. J. Med. Genet. 2023, 66, 104674. [Google Scholar] [CrossRef]
- Chronopoulos, A.; Babst, N.; Schiemenz, C.; Schutz, J.S.; Heindl, L.M.; Ranjbar, M.; Kakkassery, V. A Narrative Review—Therapy Options and Therapy Failure in Retinoblastoma. Neurosignals. 2022, 30, 39–58. [Google Scholar] [CrossRef]
- Shields, C.L.; Bas, Z.; Laiton, A.; Silva, A.M.V.; Sheikh, A.; Lally, S.E.; Shields, J.A. Retinoblastoma: Emerging concepts in genetics, global disease burden, chemotherapy outcomes, and psychological impact. Eye 2023, 37, 815–822. [Google Scholar] [CrossRef]
- Kaewkhaw, R.; Rojanaporn, D. Retinoblastoma: Etiology, Modeling, and Treatment. Cancers 2020, 12, 2304. [Google Scholar] [CrossRef]
- Munier, F.L.; Beck-Popovic, M.; Chantada, G.L.; Cobrinik, D.; Kivelä, T.T.; Lohmann, D.; Maeder, P.; Moll, A.C.; Carcaboso, A.M.; Moulin, A.; et al. Conservative management of retinoblastoma: Challenging orthodoxy without compromising the state of metastatic grace. “Alive, with good vision and no comorbidity”. Prog. Retin. Eye Res. 2019, 73, 100764. [Google Scholar] [CrossRef]
- Temming, P.; Arendt, M.; Viehmann, A.; Eisele, L.; Le Guin, C.H.D.; Schündeln, M.M.; Biewald, E.; Astrahantseff, K.; Wieland, R.; Bornfeld, N.; et al. Incidence of second cancers after radiotherapy and systemic chemotherapy in heritable retinoblastoma survivors: A report from the German reference center. Pediatr. Blood Cancer 2017, 64, 71–80. [Google Scholar] [CrossRef]
- Campeau, E.; Ruhl, V.E.; Rodier, F.; Smith, C.L.; Rahmberg, B.L.; Fuss, J.O.; Campisi, J.; Yaswen, P.; Cooper, P.K.; Kaufman, P.D. A versatile viral system for expression and depletion of proteins in mammalian cells. PLoS ONE 2009, 4, e6529. [Google Scholar] [CrossRef] [PubMed]
- Lawson, B.M.; Saktanasate, J.; Say, E.A.T.; Shields, C.L. Intravitreal chemotherapy provides control for massive vitreous seeding from retinoblastoma. J. Pediatr. Ophthalmol. Strabismus 2014, 51, e92–e94. [Google Scholar] [CrossRef] [PubMed]
- Manjandavida, F.P.; Shields, C.L. The role of intravitreal chemotherapy for retinoblastoma. Indian J. Ophthalmol. 2015, 63, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Francis, J.H.; Abramson, D.H.; Ji, X.; Shields, C.L.; Teixeira, L.F.; Schefler, A.C.; Cassoux, N.; Hadjistilianou, D.; Berry, J.L.; Frenkel, S.; et al. Risk of Extraocular Extension in Eyes With Retinoblastoma Receiving Intravitreous Chemotherapy. JAMA Ophthalmol. 2017, 135, 1426–1429. [Google Scholar] [CrossRef]
- Munier, F.L.; Gaillard, M.-C.; Balmer, A.; Beck-Popovic, M. Intravitreal chemotherapy for vitreous seeding in retinoblastoma: Recent advances and perspectives. Saudi J. Ophthalmol. 2013, 27, 147–150. [Google Scholar] [CrossRef]
- Shields, C.L.; Douglass, A.M.; Beggache, M.; Say, E.A.T.; Shields, J.A. Intravitreous Chemotherapy for Active Vitreous Seeding from Retinoblastoma: Outcomes after 192 Consecutive Injections. The 2015 Howard Naquin Lecture. Retina 2016, 36, 1184–1190. [Google Scholar] [CrossRef]
- Shields, C.L.; Lally, S.E.; Leahey, A.M.; Jabbour, P.M.; Caywood, E.H.; Schwendeman, R.; Shields, J.A. Targeted retinoblastoma management: When to use intravenous, intra-arterial, periocular, and intravitreal chemotherapy. Curr. Opin. Ophthalmol. 2014, 25, 374–385. [Google Scholar] [CrossRef]
- AlAli, A.; Kletke, S.; Gallie, B.; Lam, W.-C. Retinoblastoma for Pediatric Ophthalmologists. Asia Pac. J. Ophthalmol. 2018, 7, 160–168. [Google Scholar] [CrossRef]
- Soliman, S.E.; Racher, H.; Zhang, C.; MacDonald, H.; Gallie, B.L. Genetics and Molecular Diagnostics in Retinoblastoma—An Update. Asia Pac. J. Ophthalmol. 2017, 6, 197–207. [Google Scholar] [CrossRef]
- Soliman, S.E.; Wan, M.J.; Heon, E.; Hazrati, L.-N.; Gallie, B. Retinoblastoma versus advanced Coats’ disease: Is enucleation the answer? Ophthalmic Genet. 2017, 38, 291–293. [Google Scholar] [CrossRef] [PubMed]
- Ghiam, B.K.; Xu, L.; Berry, J.L. Aqueous Humor Markers in Retinoblastoma, a Review. Transl. Vis. Sci. Technol. 2019, 8, 13. [Google Scholar] [CrossRef] [PubMed]
- Busch, M.A.; Haase, A.; Miroschnikov, N.; Doege, A.; Biewald, E.; Bechrakis, N.E.; Beier, M.; Kanber, D.; Lohmann, D.; Metz, K.; et al. TFF1 in Aqueous Humor—A Potential New Biomarker for Retinoblastoma. Cancers 2022, 14, 677. [Google Scholar] [CrossRef] [PubMed]
- Martel, A.; Baillif, S.; Nahon-Esteve, S.; Gastaud, L.; Bertolotto, C.; Roméo, B.; Mograbi, B.; Lassalle, S.; Hofman, P. Liquid Biopsy for Solid Ophthalmic Malignancies: An Updated Review and Perspectives. Cancers 2020, 12, 3284. [Google Scholar] [CrossRef]
- Fernández-Lázaro, D.; Hernández, J.L.G.; García, A.C.; Del Castillo, A.C.; Hueso, M.V.; Cruz-Hernández, J.J. Clinical Perspective and Translational Oncology of Liquid Biopsy. Diagnostics 2020, 10, 443. [Google Scholar] [CrossRef]
- Berry, J.L.; Xu, L.; Murphree, A.L.; Krishnan, S.; Stachelek, K.; Zolfaghari, E.; McGovern, K.; Lee, T.C.; Carlsson, A.; Kuhn, P.; et al. Potential of Aqueous Humor as a Surrogate Tumor Biopsy for Retinoblastoma. JAMA Ophthalmol. 2017, 135, 1221–1230. [Google Scholar] [CrossRef]
- Im, D.H.; Pike, S.; Reid, M.W.; Peng, C.-C.; Sirivolu, S.; Grossniklaus, H.E.; Hubbard, G.B.; Skalet, A.H.; Bellsmith, K.N.; Shields, C.L.; et al. A Multicenter Analysis of Nucleic Acid Quantification Using Aqueous Humor Liquid Biopsy in Retinoblastoma: Implications for Clinical Testing. Ophthalmol. Sci. 2023, 3, 100289. [Google Scholar] [CrossRef]
- Ghose, N.; Kaliki, S. Liquid biopsy in Retinoblastoma: A review. Semin. Ophthalmol. 2022, 37, 813–819. [Google Scholar] [CrossRef]
- Zhang, Z.; Wu, H.; Chong, W.; Shang, L.; Jing, C.; Li, L. Liquid biopsy in gastric cancer: Predictive and prognostic biomarkers. Cell Death Dis. 2022, 13, 903. [Google Scholar] [CrossRef]
- Hou, Y.; Peng, Y.; Li, Z. Update on prognostic and predictive biomarkers of breast cancer. Semin. Diagn. Pathol. 2022, 39, 322–332. [Google Scholar] [CrossRef]
- Freitas, A.J.A.D.; Causin, R.L.; Varuzza, M.B.; Calfa, S.; Hidalgo Filho, C.M.T.; Komoto, T.T.; Souza, C.D.P.; Marques, M.M.C. Liquid Biopsy as a Tool for the Diagnosis, Treatment, and Monitoring of Breast Cancer. Int. J. Mol. Sci. 2022, 23, 9952. [Google Scholar] [CrossRef] [PubMed]
- Galardi, A.; Stathopoulos, C.; Colletti, M.; Lavarello, C.; Russo, I.; Cozza, R.; Romanzo, A.; Carcaboso, A.M.; Locatelli, F.; Petretto, A.; et al. Proteomics of Aqueous Humor as a Source of Disease Biomarkers in Retinoblastoma. Int. J. Mol. Sci. 2022, 23, 13458. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Xi, H.-Y.; Shao, Q.; Liu, Q.-H. Biomarkers in retinoblastoma. Int. J. Ophthalmol. 2020, 13, 325–341. [Google Scholar] [CrossRef]
- Abramson, D.H.; Piro, P.A.; Ellsworth, R.M.; Kitchin, F.D.; McDonald, M. Lactate dehydrogenase levels and isozyme patterns. Measurements in the aqueous humor and serum of retinoblastoma patients. Arch. Ophthalmol. 1979, 97, 870–871. [Google Scholar] [CrossRef] [PubMed]
- Piro, P.A., Jr.; Abramson, D.H.; Ellsworth, R.M.; Kitchin, D. Aqueous humor lactate dehydrogenase in retinoblastoma patients. Clinicopathologic correlations. Arch. Ophthalmol. 1978, 96, 1823–1825. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.-B.; Liu, X.-Q.; Li, B.; He, X.-J.; Jin, Y.-L.; Li, L.-Q.; Gao, F.; Wang, N.-L. Heat shock proteins and survivin: Relationship and effects on proliferation index of retinoblastoma cells. Histol. Histopathol. 2008, 23, 827–831. [Google Scholar] [CrossRef] [PubMed]
- Shehata, H.H.; Abou Ghalia, A.H.; Elsayed, E.K.; Ahmed Said, A.M.; Mahmoud, S.S. Clinical significance of high levels of survivin and transforming growth factor beta-1 proteins in aqueous humor and serum of retinoblastoma patients. J. AAPOS 2016, 20, 444.e1–444.e9. [Google Scholar] [CrossRef] [PubMed]
- Busch, M.; Metz, K.; Beier, M.; Biewald, E.; Dünker, N. Trefoil factor family 1 expression correlates with clinical outcome in patients with retinoblastoma. Retina 2017, 38, 2422–2428. [Google Scholar] [CrossRef]
- Hoffmann, W. Trefoil factors TFF (trefoil factor family) peptide-triggered signals promoting mucosal restitution. Cell. Mol. Life Sci. 2005, 62, 2932–2938. [Google Scholar] [CrossRef]
- Hoffmann, W. Trefoil Factor Family (TFF) Peptides and Their Diverse Molecular Functions in Mucus Barrier Protection and More: Changing the Paradigm. Int. J. Mol. Sci. 2020, 21, 4535. [Google Scholar] [CrossRef]
- Braga Emidio, N.; Brierley, S.M.; Schroeder, C.I.; Muttenthaler, M. Structure, Function, and Therapeutic Potential of the Trefoil Factor Family in the Gastrointestinal Tract. ACS Pharmacol. Transl. Sci. 2020, 3, 583–597. [Google Scholar] [CrossRef] [PubMed]
- Heuer, J.; Heuer, F.; Stürmer, R.; Harder, S.; Schlüter, H.; Braga Emidio, N.; Muttenthaler, M.; Jechorek, D.; Meyer, F.; Hoffmann, W. The Tumor Suppressor TFF1 Occurs in Different Forms and Interacts with Multiple Partners in the Human Gastric Mucus Barrier: Indications for Diverse Protective Functions. Int. J. Mol. Sci. 2020, 21, 2508. [Google Scholar] [CrossRef] [PubMed]
- Weise, A.; Dünker, N. High trefoil factor 1 (TFF1) expression in human retinoblastoma cells correlates with low growth kinetics, increased cyclin-dependent kinase (CDK) inhibitor levels and a selective down-regulation of CDK6. Histochem. Cell Biol. 2013, 139, 323–338. [Google Scholar] [CrossRef] [PubMed]
- Philippeit, C.; Busch, M.; Dünker, N. Epigenetic control of trefoil factor family (TFF) peptide expression in human retinoblastoma cell lines. Cell. Physiol. Biochem. 2014, 34, 1001–1014. [Google Scholar] [CrossRef]
- Busch, M.; Grosse-Kreul, J.; Wirtz, J.J.; Beier, M.; Stephan, H.; Royer-Pokora, B.; Metz, K.; Dunker, N. Reduction of the tumorigenic potential of human retinoblastoma cell lines by TFF1 overexpression involves p53/caspase signaling and miR-18a regulation. Int. J. Cancer 2017, 141, 549–560. [Google Scholar] [CrossRef]
- Katsha, A.; Soutto, M.; Sehdev, V.; Peng, D.; Washington, M.K.; Piazuelo, M.B.; Tantawy, M.N.; Manning, H.C.; Lu, P.; Shyr, Y.; et al. Aurora kinase A promotes inflammation and tumorigenesis in mice and human gastric neoplasia. Gastroenterology 2013, 145, 1312–1322.e8. [Google Scholar] [CrossRef] [PubMed]
- Soutto, M.; Chen, Z.; Saleh, M.A.; Katsha, A.; Zhu, S.; Zaika, A.; Belkhiri, A.; El-Rifai, W. TFF1 activates p53 through down-regulation of miR-504 in gastric cancer. Oncotarget 2014, 5, 5663–5673. [Google Scholar] [CrossRef]
- Busch, M.; Philippeit, C.; Weise, A.; Dünker, N. Re-characterization of established human retinoblastoma cell lines. Histochem. Cell Biol. 2015, 143, 325–338. [Google Scholar] [CrossRef]
- Eide, N.; Walaas, L. Fine-needle aspiration biopsy and other biopsies in suspected intraocular malignant disease: A review. Acta Ophthalmol. 2009, 87, 588–601. [Google Scholar] [CrossRef]
- Karcioglu, Z.A. Fine needle aspiration biopsy (FNAB) for retinoblastoma. Retina 2002, 22, 707–710. [Google Scholar] [CrossRef]
- Ali, M.J.; Honavar, S.G.; Vemuganti, G.K.; Singh, A.D. Fine needle aspiration biopsy of retinal tumors. Monogr. Clin. Cytol. 2012, 21, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Raval, V.; Racher, H.; Wrenn, J.; Singh, A.D. Aqueous humor as a surrogate biomarker for retinoblastoma tumor tissue. J. AAPOS 2022, 26, 137.e1–137.e5. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.J.; Smith, B.D. Evaluating the risk of extraocular tumour spread following intravitreal injection therapy for retinoblastoma: A systematic review. Br. J. Ophthalmol. 2013, 97, 1231–1236. [Google Scholar] [CrossRef] [PubMed]
- Ghassemi, F.; Shields, C.L.; Ghadimi, H.; Khodabandeh, A.; Roohipoor, R. Combined intravitreal melphalan and topotecan for refractory or recurrent vitreous seeding from retinoblastoma. JAMA Ophthalmol. 2014, 132, 936–941. [Google Scholar] [CrossRef] [PubMed]
- Francis, J.H.; Schaiquevich, P.; Buitrago, E.; Del Sole, M.J.; Zapata, G.; Croxatto, J.O.; Marr, B.P.; Brodie, S.E.; Berra, A.; Chantada, G.L.; et al. Local and systemic toxicity of intravitreal melphalan for vitreous seeding in retinoblastoma: A preclinical and clinical study. Ophthalmology 2014, 121, 1810–1817. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.J.; Smith, B.D.; Mohney, B.G. Ocular side effects following intravitreal injection therapy for retinoblastoma: A systematic review. Br. J. Ophthalmol. 2014, 98, 292–297. [Google Scholar] [CrossRef] [PubMed]
- Uner, O.E.; Ulrich, B.C.; Hubbard, G.B. Potential of Aqueous Humor as a Surrogate Tumor Biopsy for Retinoblastoma. JAMA Ophthalmol. 2018, 136, 597–598. [Google Scholar] [CrossRef]
- Liu, W.; Luo, Y.; Dai, J.; Yang, L.; Huang, L.; Wang, R.; Chen, W.; Huang, Y.; Sun, S.; Cao, J.; et al. Monitoring Retinoblastoma by Machine Learning of Aqueous Humor Metabolic Fingerprinting. Small Methods 2022, 6, e2101220. [Google Scholar] [CrossRef]
- Berry, J.L.; Xu, L.; Polski, A.; Jubran, R.; Kuhn, P.; Kim, J.W.; Hicks, J. Aqueous Humor Is Superior to Blood as a Liquid Biopsy for Retinoblastoma. Ophthalmology 2020, 127, 552–554. [Google Scholar] [CrossRef]
- Yi, J.; Ren, L.; Li, D.; Wu, J.; Li, W.; Du, G.; Wang, J. Trefoil factor 1 (TFF1) is a potential prognostic biomarker with functional significance in breast cancers. Biomed. Pharmacother. 2020, 124, 109827. [Google Scholar] [CrossRef]
- Schulten, H.-J.; Bangash, M.; Karim, S.; Dallol, A.; Hussein, D.; Merdad, A.; Al-Thoubaity, F.K.; Al-Maghrabi, J.; Jamal, A.; Al-Ghamdi, F.; et al. Comprehensive molecular biomarker identification in breast cancer brain metastases. J. Transl. Med. 2017, 15, 269. [Google Scholar] [CrossRef] [PubMed]
- Gonzaga, I.M.; Soares Lima, S.C.; Nicolau, M.C.; Nicolau-Neto, P.; da Costa, N.M.; de Almeida Simão, T.; Hernandez-Vargas, H.; Herceg, Z.; Ribeiro Pinto, L.F. TFF1 hypermethylation and decreased expression in esophageal squamous cell carcinoma and histologically normal tumor surrounding esophageal cells. Clin. Epigenet. 2017, 9, 130. [Google Scholar] [CrossRef] [PubMed]
- Shimura, T.; Dayde, D.; Wang, H.; Okuda, Y.; Iwasaki, H.; Ebi, M.; Kitagawa, M.; Yamada, T.; Yamada, T.; Hanash, S.M.; et al. Novel urinary protein biomarker panel for early diagnosis of gastric cancer. Br. J. Cancer 2020, 123, 1656–1664. [Google Scholar] [CrossRef]
- Elnagdy, M.H.; Farouk, O.; Seleem, A.K.; Nada, H.A. TFF1 and TFF3 mRNAs Are Higher in Blood from Breast Cancer Patients with Metastatic Disease than Those without. J. Oncol. 2018, 2018, 4793498. [Google Scholar] [CrossRef] [PubMed]






| TFF1 Expressed n (%) | TFF1 Not Expressed n (%) | N | |
|---|---|---|---|
| Patient’s | 7 (87.5) | 1 (12.5) | 8 |
| Sex | |||
| female | 2 (28.6) | 0 (0) | 2 |
| m | 5 (71.4) | 1 (100) | 6 |
| ICRB stage | |||
| D | 1 (14.3) | 0 (0) | 1 |
| E | 4 (57.1) | 1 (100) | 5 |
| na | 2 (28.6) | 0 (0) | 2 |
| Laterality | |||
| unilateral | 7 (100) | 1 (100) | 8 |
| bilateral | 0 (0) | 0 (0) | 0 |
| Age at diagnosis | |||
| <18 month | 0 (0) | 1 (100) | 1 |
| 18–36 month | 6 (85.7) | 0 (0) | 6 |
| >36 month | 1 (14.3) | 0 (0) | 1 |
| Tumor volume | |||
| <1 cm3 | 1 (14.3) | 0 (0) | 1 |
| 2–3 cm3 | 2 (28.6) | 0 (0) | 2 |
| >3 cm3 | 4 (57.1) | 1 (100) | 5 |
| Optic nerve invasion | |||
| none | 5 (71.4) | 1 (100) | 6 |
| p-laminar | 2 (28.6) | 0 (0) | 2 |
| post-laminar | 0 (0) | 0 (0) | 0 |
| Choroid invasion | |||
| none | 7 (100) | 1 (100) | 8 |
| invasion | 0 (0) | 0 (0) | 0 |
| Case | Sex | Age at Diagnosis (Month) | Laterality | ICRB Stage | Tumor Size (mm) | Enucleation | Optic Nerve Invasion (MRI) | Choroid Invasion (MRI) | RB1 Mutation | Sample Number | AH TFF1 (pg/mL) | Serum TFF1 (pg/mL) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T24 # | m | t: 23 r: 148 | b | ri: B le: E | ri: 4.5 le: >10 | le: PE | no | no | yes | 1 2 3 | 0 0 0 | 9.73 9.97 11.12 |
| T25 | f | 18 | u | D | 8.7 | no | no | yes | no | 1 2 3 4 5 6 | 0 0 0 0 0 0 | 11.55 0 10.6 0 0 0 |
| T26 | m | 14 | b | D | 9 (both) | ri: no le: SE | no | ri: no le: yes | yes | 1 2 3 | 0 0 0 | 0 0 0 |
| T28 # | f | t: 23 r: 51 r2: 56 | b | E | ri: 12 le: 20 | ri: no le: PE | ri: no le: yes | ri: no le: yes | yes | 1 2 3 4 | 118.98 124.37 95.9 119.41 | 0 0 0 0 |
| T33 | m | 24 | u | D | n/a | no | n/a | n/a | n/a | 1 2 3 4 5 6 7 8 9 10 11 | 180.21 54.28 0 0 0 0 0 0 0 0 0 | 10.65 9.23 0 0 0 9.33 0 0 9.83 10.14 0 |
| T39 | f | 26 | b | ri: E le: D | ri: 22 le: 7 | ri: SE le: no | ri: yes le: no | ri: yes le: no | yes | 1 2 3 | 0 0 0 | 9.93 0 9.98 |
| T44 | m | 62 | u | C | 8 | no | no | no | n/a | 1 * 2 | 340.58 0 | 10.57 9.84 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Busch, M.A.; Haase, A.; Alefeld, E.; Biewald, E.; Jabbarli, L.; Dünker, N. Trefoil Family Factor Peptide 1—A New Biomarker in Liquid Biopsies of Retinoblastoma under Therapy. Cancers 2023, 15, 4828. https://0-doi-org.brum.beds.ac.uk/10.3390/cancers15194828
Busch MA, Haase A, Alefeld E, Biewald E, Jabbarli L, Dünker N. Trefoil Family Factor Peptide 1—A New Biomarker in Liquid Biopsies of Retinoblastoma under Therapy. Cancers. 2023; 15(19):4828. https://0-doi-org.brum.beds.ac.uk/10.3390/cancers15194828
Chicago/Turabian StyleBusch, Maike Anna, André Haase, Emily Alefeld, Eva Biewald, Leyla Jabbarli, and Nicole Dünker. 2023. "Trefoil Family Factor Peptide 1—A New Biomarker in Liquid Biopsies of Retinoblastoma under Therapy" Cancers 15, no. 19: 4828. https://0-doi-org.brum.beds.ac.uk/10.3390/cancers15194828