A Drug Content, Stability Analysis, and Qualitative Assessment of Pharmacists’ Opinions of Two Exemplar Extemporaneous Formulations
Abstract
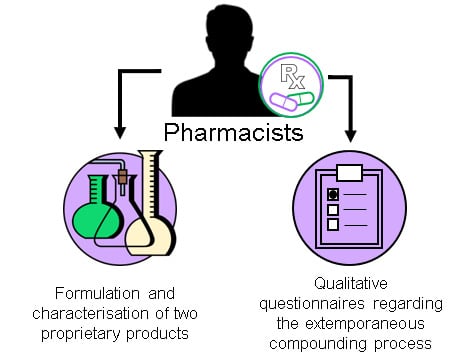
:1. Introduction
2. Results
2.1. Pharmaceutical Analysis of Omeprazole and Amlodipine
2.2. Preparation of Formulations of Omeprazole and Amlodipine by Pharmacists: Drug Content, Stability Studies and Analysis of Particle Size Distribution
2.3. Assessing Efficacy of Antimicrobial Preservation
2.4. Assessing Pharmacists’ Opinions
‘…crushing granules was difficult and they kept escaping from the mortar’.(Pharmacist 10)
‘Extremely time consuming due to the relative difficulty in grinding/crushing the small and hard granules within the capsule’.(Pharmacist 5)
‘It was likely some of the active ingredient was lost during the crushing process due to the size of the granules within each capsule’.(Pharmacist 2)
‘Tablets were easier to crush than the omeprazole granules’.(Pharmacist 5)
‘Tablets were more easily crushed in this case’.(Pharmacist 4)
‘Crushing the tablets uniformly was time-consuming’.(Pharmacist 10)
3. Discussion
3.1. Preparation and Characterisation of Omeprazole and Amlodipine Formulations
3.2. Pharmacists’ Opinions and Confidence Surrounding the Perceived Complexity of the Extemporaneous Compounding Process
4. Materials and Methods
4.1. Chemicals
4.2. Pharmaceutical Analysis of Omeprazole and Amlodipine
4.3. Preparation of Omeprazole and Amlodipine Formulations
4.4. Drug Quantification and Stability Profile
4.5. Particle Size
4.6. Antimicrobial Preservation
4.7. Assessing Pharmacists’ Opinions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Giam, J.A.; McLachlan, A.J. Extemporaneous product use in paediatric patients: A systematic review. Int. J. Pharm. Pract. 2008, 16, 3–10. [Google Scholar] [CrossRef]
- NHS Pharmaceutical Quality Assurance Committee. A Standard Protocol for Deriving and Assessment of Stability Part 3—Oral Liquid Medicines (Solutions, Emulsions, Suspensions and Syrups). 2014. Available online: https://www.sps.nhs.uk/articles/a-standard-protocol-for-deriving-and-assessment-of-stability-part-3-oral-liquid-medicines-solutions-emulsions-suspensions-and-syrups-edition-1-august-2014/ (accessed on 12 July 2019).
- McCague, P.; McElnay, J.; Donnelly, R.F. What are your views on specials and extemporaneous medicines preparation? Pharm. J. 2012. Available online: https://www.pharmaceutical-journal.com/news-and-analysis/what-are-your-views-on-specials-and-extemporaneous-medicines-preparation/11102745.article (accessed on 1 August 2019).
- Langley, C.A. Pharmacy legislation: Public protector or professional hindrance? Med. Law Rev. 2014, 22, 87–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McNally, M.J.; Barry, J.G.; Donnelly, R.F. Development and validation of procedures for assessment of competency of non-pharmacists in extemporaneous dispensing. Int. J. Pharm. Pract. 2009, 17, 67–71. [Google Scholar] [CrossRef]
- Conroy, S. Making paediatric medicines work. Pharm. J. 2008, 2–4. Available online: https://www.pharmaceutical-journal.com/news-and-analysis/fip-2008-making-paediatric-medicines-work/10040952.article (accessed on 24 July 2019).
- Chowdhury, T.; Taylor, K.M.G.; Harding, G. Teaching Extemporaneous Preparation in UK Schools of Pharmacy. Pharm. Educ. 2003, 3, 229–236. [Google Scholar] [CrossRef]
- Neill, H. Do not be afraid to ask for help (letter). Pharm. J. 2003, 270. Available online: https://www.pharmaceutical-journal.com/pj-online-pj-letters-dispensing/20008847.article (accessed on 12 July 2019).
- Royal Pharmaceutical Society. Good Practice Guidance on: The Procurement and Supply of Pharmaceutical Specials Update June 2011. Available online: https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Support/toolkit/good-practice-guidance-proc-supply-pharm-specials-%287%29.pdf (accessed on 12 August 2019).
- Pappas, A. Extemporaneous Dispensing: Opinions of Victorian Community Pharmacists. Aust. J. Hosp. Pharm. 1999, 29, 196–201. [Google Scholar] [CrossRef]
- Van Der Pol, R.J.; Smits, M.J.; Van Wijk, M.P.; Omari, T.I.; Tabbers, M.M.; Benning, M.A. Efficacy of proton-pump inhibitors in children with gastroesophageal reflux disease: A systematic review. Pediatrics 2011, 127, 925–935. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, R. Is extemporaneous dispensing really in the best interest of patients? Pharm. J. 2008. Available online: https://www.pharmaceutical-journal.com/news-and-analysis/opinion/comment/is-extemporaneous-dispensing-really-in-the-best-interest-of-patients/10007271.article (accessed on 12 August 2019).
- Pharmaceutical Society of Northern Ireland. Professional Standards and Guidance for the Sale and Supply of Medicines. 2016. Available online: https://www.psni.org.uk/wp-content/uploads/documents/313/standards_on_sale_and_supply_of_medicines.pdf (accessed on 15 July 2019).
- Hough, R. Guidance on extemp preparations. Indep. Community Pharm. 2014. Available online: https://www.independentpharmacist.co.uk/guidance-on-extemp-preparations (accessed on 8 July 2019).
- Jackson, M.; Lowey, A. Handbook of Extemporaneous Preparation, 1st ed.; Pharmaceutical Press: London, UK, 2010. [Google Scholar]
- Rosemont Pharmaceuticals 2018. Available online: https://www.rosemontpharma.com/ (accessed on 24 July 2019).
- Saidum, S.; Pratheepawanit, N. Behaviour and understanding parents about dry syrup antibiotic use. Thai. J. Hosp. Pharm. 2010, 19, S79–S89. [Google Scholar]
- Helin-Tanninen, M.; Autio, K.; Keski-Rahkonen, P.; Naaranlahti, T.; Järvinen, K. Comparison of six different suspension vehicles in compounding of oral extemporaneous nifedipine suspension for paediatric patients. Eur. J. Hosp. Pharm. 2012, 19, 432–437. [Google Scholar] [CrossRef]
- Corral, L.G.; Post, L.S.; Montville, T.J. Antimicrobial Activity of Sodium Bicarbonate. J. Food Sci. 1988, 53, 981–982. [Google Scholar] [CrossRef]
- Rowe, R.; Sheskey, P. Handbook of Pharmaceutical Excipients, 7th ed.; Pharmaceutical Press: London, UK, 2012. [Google Scholar]
- The International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use. ICH Topic Q 2 (R1) Validation of Analytical Procedures: Text and Methodology. Int. Conf. Harmon. 1994, 17. Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/ich-q-2-r1-validation-analytical-procedures-text-methodology-step-5_en.pdf (accessed on 17 September 2019).


| Drug | Slope | y-Intercept | R2 | LoD (mcg/mL) | LoQ (mcg/mL) |
|---|---|---|---|---|---|
| Omeprazole | 62.5 | −17.28 | 0.998 | 3.47 | 10.50 |
| Amlodipine | 39.18 | −8.53 | 0.999 | 0.85 | 2.59 |
| Pharmacist ID | Omeprazole | Amlodipine | ||
|---|---|---|---|---|
| Concentration of Product (mg/mL) | Percentage of Theoretical Drug Content (%) | Concentration of Product (mg/mL) | Percentage of Theoretical Drug Content (%) | |
| 1 | 1.81 | 90.61 | 0.95 | 94.52 |
| 2 | 1.85 | 92.75 | 1.18 | 118.36 |
| 3 | 1.87 | 93.62 | 1.17 | 116.57 |
| 4 | 1.85 | 92.61 | 1.20 | 120.09 |
| 5 | 1.73 | 86.47 | 0.85 | 85.05 |
| 6 | 1.79 | 89.60 | 0.85 | 84.94 |
| 7 | 1.85 | 92.61 | 1.05 | 104.52 |
| 8 | 1.87 | 93.74 | 0.86 | 85.63 |
| 9 | 1.80 | 90.15 | 0.73 | 72.63 |
| 10 | 1.26 | 62.84 | 0.99 | 98.68 |
| Mean Initial Bacterial Count | Log Reduction of Bacterial Count | |||
|---|---|---|---|---|
| Bacterial Species | Omeprazole | Amlodipine | Omeprazole | Amlodipine |
| Pseudomonas aeruginosa | 3.87 × 106 | 1.88 × 106 | 6.59 | 6.27 |
| Escherichia coli | 3.01 × 105 | 1.88 × 106 | 5.48 | 6.27 |
| Staphylococcus aureus | 2.37 × 106 | 4.58 × 105 | 6.37 | 5.66 |
| Statement | Median (IQR) | p * |
|---|---|---|
| Overall level of confidence extemporaneously preparing the omeprazole suspension. | 3.00 (2.75–4.00) | 0.16 |
| Overall level of confidence extemporaneously preparing the amlodipine suspension. | 4.00 (2.75–4.00) | |
| Level of complexity preparing the omeprazole suspension. | 2.50 (2.00–3.25) | 0.66 |
| Level of complexity preparing the amlodipine suspension. | 2.50 (2.00–3.25) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kirkby, M.; Moffatt, K.; Rogers, A.M.; McCague, P.J.; McElnay, J.C.; Quinn, C.; McCullough, L.A.; Barry, J.; Donnelly, R.F. A Drug Content, Stability Analysis, and Qualitative Assessment of Pharmacists’ Opinions of Two Exemplar Extemporaneous Formulations. Molecules 2020, 25, 3078. https://0-doi-org.brum.beds.ac.uk/10.3390/molecules25133078
Kirkby M, Moffatt K, Rogers AM, McCague PJ, McElnay JC, Quinn C, McCullough LA, Barry J, Donnelly RF. A Drug Content, Stability Analysis, and Qualitative Assessment of Pharmacists’ Opinions of Two Exemplar Extemporaneous Formulations. Molecules. 2020; 25(13):3078. https://0-doi-org.brum.beds.ac.uk/10.3390/molecules25133078
Chicago/Turabian StyleKirkby, Melissa, Kurtis Moffatt, Aoife M. Rogers, Paul J. McCague, James C. McElnay, Caoimhe Quinn, Lezley Ann McCullough, Johanne Barry, and Ryan F. Donnelly. 2020. "A Drug Content, Stability Analysis, and Qualitative Assessment of Pharmacists’ Opinions of Two Exemplar Extemporaneous Formulations" Molecules 25, no. 13: 3078. https://0-doi-org.brum.beds.ac.uk/10.3390/molecules25133078